ROOT CANAL TREATMENT
The name Root Canal sends chills down the spine of most that have heard about it or have experienced it in the past. The reason is that either they have had a bad experience with this modality of treatment or have heard horrifying stories.

Technology has changed every aspect of life and how could dentistry or for that matter root canal treatment be left behind. There have been tremendous advances in the techniques and the instruments used in root canal procedures which have made it a completely painless procedure. We use the most modern instruments and equipments available in the field of endodontics which gives us predictably good results in less time. We use the state of the art Rotary nickel-titanium preparation instruments, X Smart, Path Files, Glyde, Apex Locator II, Activator to clean and prepare the canals. Here’s about it…Be informed!
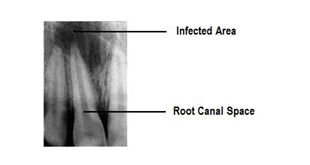
When the cavity in the tooth spreads beyond the two layers- enamel and dentin, it involves pulp. Once infected the pulp tissue cannot be brought back to health by medications or any other procedure and the only treatment of such a tooth is either root canal treatment or removal. Teeth that have root canal problems are generally painful. Decomposing nerves and blood vessels create gases that expand and are locked into the pulp chamber and root canals. They cause pressure which results in pain. The pain can also be in response to temperature changes, especially hot drinks, or can be spontaneous, very severe, and even throbbing in nature. The tooth may be tender on chewing.
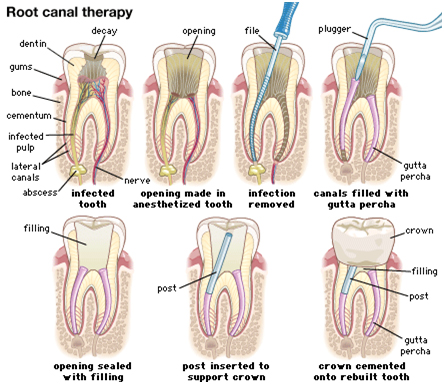
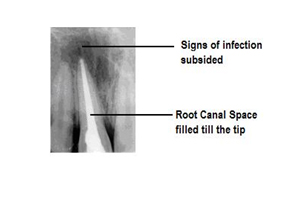
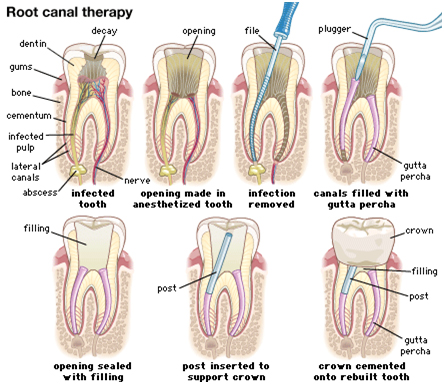
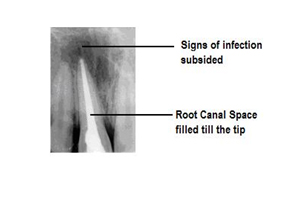
The procedure of root canal generally begins with an anesthetic shot so that the tooth does not hurt throughout the procedure. The anesthesia used is a local one hence the patient is awake, conscious and in full control of his motor and sensory reflexes. After the anesthesia has acted completely the dentist then drills to first clean up the decayed part of the tooth structure and then to gain access to the root canal through the pulp chamber. The infected pulp tissue is then cleaned right unto the tip of the root using rotary or hand files and an apex locator. The dentist may even take x-rays to check the root length. After complete cleaning of the canals is achieved the space created by the removal of the pulp tissue is then filled up using a sealer and gutta-percha points. The excess gutta-percha is then sheared off with a hot instrument and the pulp chamber is then filled with a temporary filling.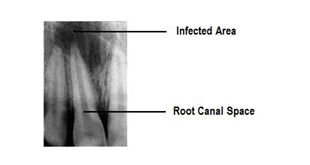
The dentist my reduce the tooth so that it is not in contact with the opposing tooth to prevent it from biting trauma immediately after the root canal treatment. The tooth is expected to be slightly painful after the treatment for a couple of days which is generally controlled using pain killers
POST AND CORE TREATMENT
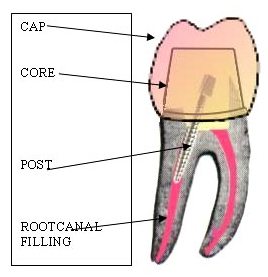
If the amount of healthy tooth structure available is not satisfactory to support a cap then an additional step of post and core may be suggested after root canal treatment.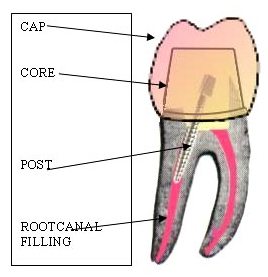
Post placement involves the cementation of a metallic or a glass-fiber pin in the root canal and building up the permanent filling around it. Thus the post provides for additional anchorage to hold the permanent filling material. Alternatively the dentist may advice a cast post and core where the post and the core(filling) is fabricated in metal by casting procedure on a model made from an impression of the affected tooth. The post is completely enclosed from all sides and does not contact any living tissue so it is completely safe and a documented procedure to salvage a badly mutilated tooth.
CROWN REHABILITATION
After a certain period endodontically treated tooth becomes dehydrated and due to this they become brittle. Fractures of Root canal treated teeth increase considerably in the posterior dentitionwhen cuspal protection is not provided by a crown . Moreover Anteriorly, the tooth may become discolored. So every Root Canal Treated tooth should receive a Crown or commonly called as a cap. Special Cases It often requires special instruments and magnification in order to see it accessory canals (most commonly found in first maxillary molars; an average of 76% up to 96% of such teeth with the presence of an MB2 canal). If any tooth may have more than one canal, it also has to be prepared while performing the root canal. Fortunately, a specialist can often re-treat and definitively heal up these teeth, often years after the initial root canal procedure. However, the survival or functionality of the endodontically-treated tooth is currently the emerging aspect of endodontic treatment outcome, rather than healing. Properly restored tooth following root canal therapy yields long-term success rates near 98-99%. Endodontically treated teeth are prone to extraction mainly due to non-restorable carious destruction and to a lesser extent to endodontic-related reasons such as endodontic failure, vertical root fracture (VRF), or perforation (procedural error).SYSTEMIC ISSUES
An infected tooth may endanger other parts of the body. People with special vulnerabilities, such as prosthetic joint replacement or valve prolapse , may need to take antibiotics to protect from infection spreading during dental procedures. Both endodontic therapy and tooth extraction can lead to subsequent jaw bone infection. The American Dental Association (ADA) asserts that any risks can be adequately controlled.COMMON SYMPTOMS REQUIRING AN RCT:
- Severe tooth pain, typically relieved by cold water and increases with the intake of hot liquids.
- Pain worsens when you lie down and reduces when you sit up.
- Pain stays for a long time after consuming cold things.
- Swelling around the tooth.
- Constant tooth pain
- Pain when chewing.
- Tooth pain referred to head and ears as well.
- Tooth sensitivity on consuming sweets.
WHY MAY ENDODONTIC DISEASE CAUSE SWELLING?
When the pulp tissue becomes severely diseased and necrotic, the resultant infection can spread from inside the tooth into the adjacent bone and soft tissues. As a result, swelling can occur in the tissues immediately surrounding the tooth. If this situation is not treated and the disease process is not kept under control by the body’s defences, the infection can begin to spread into other tissue spaces, such as those around the eye or in the neck. In some situations, this can become a serious medical emergency.ROOT CANAL RETREATMENT
Can an Endodontically Failing Tooth Be Retreated? Even when pain and/or swelling is present, the majority of failing endodontically-treated teeth can be successfully retreated in today’s world of clinical possibility. By using scientific information gathered from research and clinical studies, clinicians have developed better endodontic concepts, materials, and techniques. Additionally, there are now better-trained general dentists and specialists alike. All of these factors translate into improved care for patients. The significant technological breakthroughs that benefit both doctors and patients in endodontic retreatment include:- Magnification glasses, fibre optic lighting sources, headlamps, have significantly improved vision and hence elevated treatment success.
- Ultrasonic devices allow doctors to more efficiently and completely remove old root canal filling materials and other intra-canal obstructions so that teeth may be successfully retreated.
- Computer digital radiography technology allows the doctor to better diagnose, visualize, and treat root canal disease. Additionally, this technology significantly reduces radiation exposure to the patient
- Improved instruments, better materials for filling and repairing canals, and innovative new technologies have all contributed to significantly improved retreatment success.
WHAT IS SURGICAL ROOT CANAL TREATMENT (SRCT)?
Surgical root canal treatment is a procedural effort in which it is necessary to elevate a small flap of tissue adjacent to the involved tooth in order to gain access to and treat root canal disease. Surgical root canal treatments are usually minor, in-office procedures performed under local anaesthesia. Once the pathological area is exposed, the doctor performs a “curettage” to remove the diseased tissue from around the root. This is usually followed by an “apicoectomy,” a procedure in which the diseased portion of the root is removed. A small filling is then usually placed to seal the remaining portion of the root. Surgical root canal treatment will oftentimes result in a good long-term prognosis for the tooth if the cause of pathology can be effectively eliminated. Unfortunately, on occasion, retreatment efforts may not be possible or cost-effective and extraction may be the only alternative. However, saving a tooth that has been previously treated endodontically and is failing is usually possible, can be very predictable, and is typically the most conservative option for the patient Alternatives To Root Canal Treatment – The only alternative to root canal treatment is the extraction of the problematic tooth. It is wise to consider all of the implications of losing a tooth before having it removed. The decision should not be made hastily or because the tooth is painful. If pain is present and the dentist thinks that the tooth can be saved, the discomfort can first be relieved and then the alternatives explored.The usual alternatives that a patient has after tooth extraction are:- A restored dental implant. (BEST) This restoration involves a surgical procedure to insert the dental implant into the bone, a healing phase of several months, and a final restorative phase, which is similar to having a single tooth crown. Significant time and laboratory costs are involved.
- A fixed bridge. (Good) Fabricating a fixed bridge requires cutting down (“preparing”) the teeth next to the missing tooth so that they can receive the artificial crowns that support the replacement tooth. These teeth must be strong and healthy if they are to be effective bridge supports. Preparing the teeth for crowns could have a detrimental effect on their pulp health, depending on a variety of factors. This possibility needs to be discussed and factored into your decision. Fixed bridges may take multiple appointments to complete and have significant associated costs.
- A removable partial denture. (Damaging) These appliances restore function and esthetics and can be inserted into the mouth and removed at will. Although many teeth are successfully replaced with removable prosthetic appliances, patients may initially find them cumbersome. Removable partial dentures may also temporarily alter phonetics as well as place unfavourable forces on the supporting teeth and soft tissues. There may be significant costs associated with this restoration.
